(By Department of Cardiology)The 68th Annual Scientific Session of the American Heart Association (ACC 2019) recently opened at the Ernest N. Morial Convention Center in New Orleans. A single-center retrospective study by Professor Ping Zhang's team at Beijing Tsinghua Changgung Hospital, which provides an in-depth summary of the genetic and clinical characteristics of Chinese patients with congenital long QT syndrome (LQTS), was selected as the best wall paper at the ACC Annual Meeting, having previously won the 2018 ACC Asia Poster Winner Award.
Congenital long QT syndrome (LQTS) is an inherited ion channel disease. The electrocardiogram reflects a prolonged QT interval, which is prone to trigger Torsade de pointes (Tdp), which leads to malignant ventricular arrhythmias such as ventricular fibrillation, syncope and even sudden death. In particular, the disease is one of the most common causes of sudden death in young adults, causing great family and social burdens. At present, clinical studies on LQTS are mainly from western countries, and there are no large-sample clinical studies on LQTS in China. The prevalence of congenital LQTS in the United States is about 1:2000, and there is no statistical data available in China. Around 3000-4000 sudden cardiac deaths in the United States each year are caused by LQTS, especially in children and young adults, which has a great impact on families and society. As a large country with a large population base, China is roughly estimated to have millions of LQTS patients. Therefore, there is an urgent need to summarize the genetic and clinical characteristics of LQTS patients in China to provide useful assistance in the diagnosis, risk assessment and treatment of LQTS.
This study by Professor Ping Zhang's team yielded the important result that type 2 long QT syndrome is the most common LQTS subtype in Chinese, and some patients have multiple LQTS gene mutations. Different subtypes of LQTS patients have different triggers for cardiac events and different risks of cardiac events, and beta blockers can significantly decrease the risk and improve the prognosis of cardiac events. This study is of great value for the diagnosis and treatment of LQTS.
News Link:
The study included a total of 87 patients with a clinical diagnosis of LQTS between 2006 and 2018(60 families). All patients underwent whole-exon sequencing to identify the patient's pathogenic genes, and the results were verified by Sanger method. Female patients accounted for 63% of the cohort, with an average QTc interval of 525.11 + 77.48 MS and an average Schwartz score of 4.62 + 1.39. Among them, 61 (70%) patients had cardiac events, and the age of the first cardiac event was 18.08 + 1.86 years old.
All patients underwent genetic testing, of which 74 were initially identified as carrying disease-causing or potentially disease-causing mutations (13 KCNQ1, 45 KCNH2, 6 SCN5A, 3 KCNJ2, 1 KCNE1, 4 AKAP9 and 2 KCNJ5). The remaining 14 patients had polygenic mutations (LQTMs). A total of 63 mutated loci (9 KCNQ1, 27 KCNH2, 3 SCN5A, 3 KCNJ2, 1 KCNE1, 3 AKAP9 and 1 KCNJ5) were detected, of which 25 sites have not been reported previously.

Genotype distribution characteristics of LQTS patients
Different subtypes of LQTS patients have different causes of cardiac events. Patients with LQT1 occurs primarily during exercise or stress (99%). Patients with LQT2 had relatively diverse triggers, including agitation (23%), sound stimulation (19%), arousal (16%), fatigue (16%), urination (6%), fever (3%), hunger (3%), postural changes (10%), and in women, cardiac events occurred partially during menstruation (9%) and postpartum (4.5%). Patients with LQT3 have a predominantly resting and sleep onset. Survival analysis showed that patients with LQTM had a relatively poor prognosis.

Different triggers of disease in LQTS patients
In terms of treatment, 51 (59%) patients were treated with beta blockers. During the mean follow-up period of 7.14 + 3.12 years, the average annual cardiac event load of patients was significantly lower after drug treatment than before (1.29 + 1.83 vs. 0.16 + 0.36, P < 0.0001).
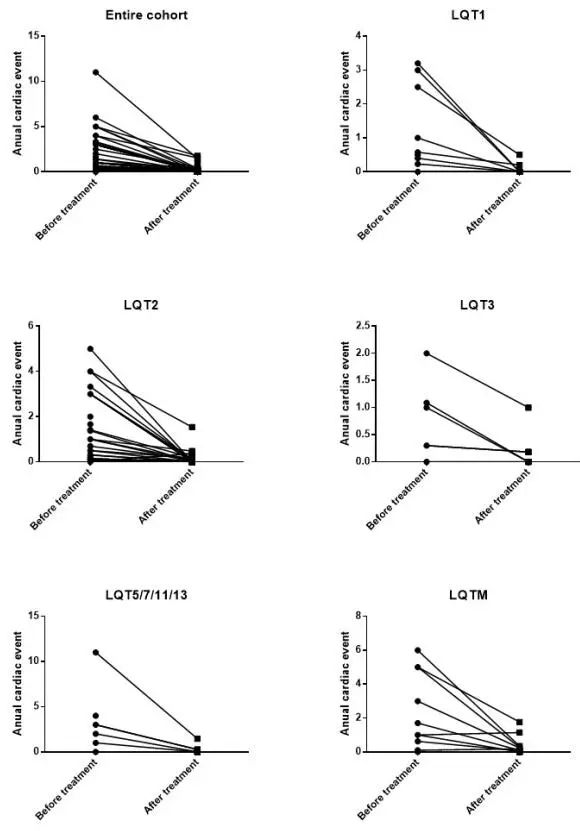
Comparison of cardiac event load before and after treatment.(Reviewer Yuan Yuan)